Creating stem cells from minipigs offers promise for improved treatments

A breed of pigs called Wisconsin Miniature Swine — created by a team of UW–Madison scientists — will help researchers better model and understand human diseases. Photo: Jeff Miller
Cells from miniature pigs are paving the way for improved stem cell therapies.
A team led by University of Wisconsin–Madison Stem Cell & Regenerative Medicine Center researcher Wan-Ju Li offers an improved way to create a particularly valuable type of stem cell in pigs – a cell that could speed the way to treatments that restore damaged tissues for conditions from osteoarthritis to heart disease in human patients.
In a study published in Scientific Reports, Li’s team also provides insights into the reprogramming process that turns cells from one part of the body into pluripotent stem cells, a type of building block cell that can transform into any type of tissue. These new insights will help researchers study treatments for a wide range of diseases.
The researchers turned to pigs, a well-established animal model for potential human treatments, because translating research to improve human health is deeply important to Li, a professor of Orthopedics and Rehabilitation and Biomedical Engineering. He has spent much of his career studying cartilage and bone regeneration to develop innovative therapies to help people.
Li and members of his Musculoskeletal Biology and Regenerative Medicine Laboratory obtained skin cells from the ears of three different breeds of miniature pigs — Wisconsin miniature swine, Yucatan miniature swine and Göttingen minipigs.
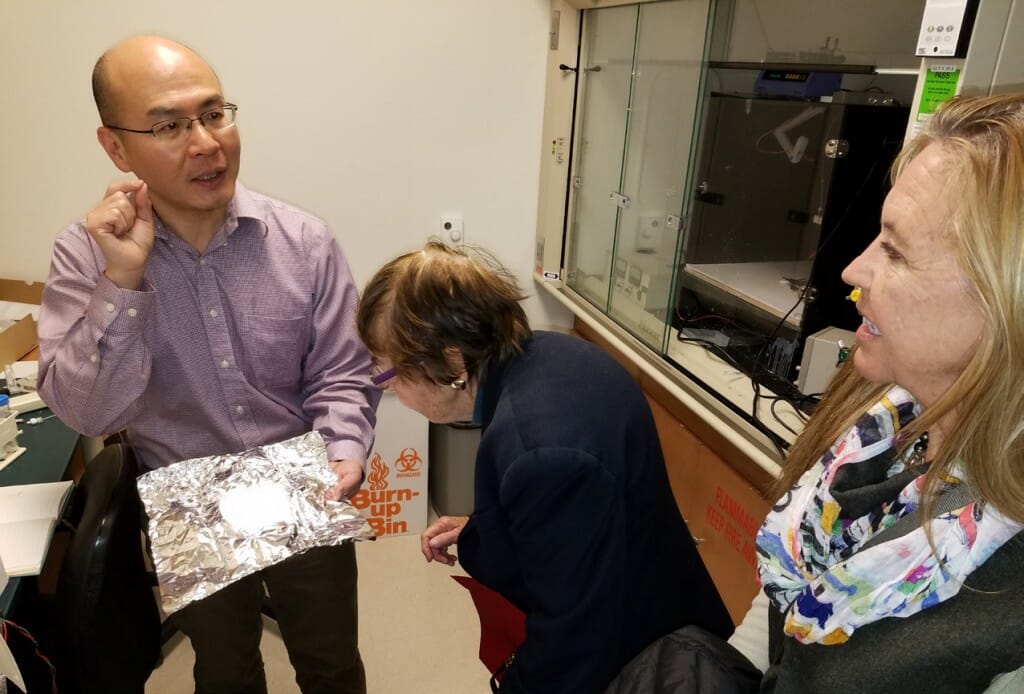
University of Wisconsin–Madison Stem Cell & Regenerative Medicine Center researcher Wan-Ju Li (left) shows a collagen fiber sample to Gwen Plunkett and Karen Plunkett. Funding from the Plunkett Family Foundation has contributed to research on cartilage repair therapies in UW–Madison’s Musculoskeletal Research Program.
The researchers reprogrammed the cells to create induced pluripotent stem cells and demonstrated that they have the capacity to become different types of tissue cells. Pluripotent stem cells are the body’s master cells, and they are invaluable to medicine since they can be used for the regeneration or repair of damaged tissues.
Findings of this study suggest that the miniature pig is a promising animal model for pre-clinical research. The team plans to use the established pig model to reproduce their recent findings of cartilage regeneration in rats as reported in Science Advances. Regenerating cartilage in animals even more alike to humans moves science one step closer to helping patients experiencing joint diseases such as osteoarthritis.
“In successfully developing induced pluripotent stem cells from three different breeds of minipigs, we learned we can take somatic skin cells from these pigs that we programmed ourselves and then inject them back into the same animal to repair cartilage defects,” says Li. “Or we can create induced pluripotent stem cells from the skin cell that carried the gene causing cartilage diseases such as chondrodysplasia and put that into the culture dish and use that as a disease model to study disease formation.”
Li says the approach can be applied to regenerative therapies targeting any organ or tissue.
The team also found that a particular protein complex involved in managing the way genes are expressed, and tied to cellular growth and survival, could influence how efficiently induced pluripotent stem cells are generated. “While we successfully created induced pluripotent stem cells from the three different strains of pig, we noticed that some pigs had a higher reprogramming efficiency,” says Li. “So, the second part of our findings, which is significant in biology, is understanding how these differences occur and why.”
These findings, he says, may directly translate to understanding differences in the effectiveness of induced pluripotent stem cell generation between individual people — one study has shown cellular reprogramming efficiency varying by age and ancestry — and lead to better tailored therapies.
“I want to make sure that our findings in stem cell research can be used to help people,” says Li. “I just feel this internal drive to study this area and I feel good knowing this model carries significant weight in terms of its potential for translational stem cell research and the development of therapeutic treatments.”
Interest in moving these treatments forward has grown, and while the study was funded in part by the National Institutes of Health, Li also received support from the Milwaukee-based Plunkett Family Foundation through their donation to the UW Stem Cell & Regenerative Medicine Center. After hearing of Li’s research, Gwen Plunkett and her daughter Karen visited Li’s lab in 2019 to learn more. They were inspired to support research into stem cells for cartilage regeneration.
“Innovation in medicine sparks critical change, for the world and the survival of our species, and the Plunkett Family mission is to be a catalyst in stem cell and regenerative medicine research,” says Karen Plunkett.
The donation was profoundly impactful, says Li, allowed him to further his goal of using stem cells to help patients living with osteoarthritis and other joint diseases — many of whom write his lab regularly in hope of finding a clinical trial opportunity.
“I have to keep saying, ‘Wait for another two, three years, maybe we’ll be ready for a clinical trial,’” Li says. “But for me, it’s time to move on and really do our larger animal studies to fulfill our promise. At least that way, I can fill the gap between the lab and clinical trials as the larger animals must be studied before you go into a clinical trial.”
This research was supported by grants from the National Institutes of Health (R01 AR064803), the Plunkett Family Foundation and UW Carbon Cancer Center.
Tags: animal research, health, stem cells



