Center helps make radiation treatment for cancer safer
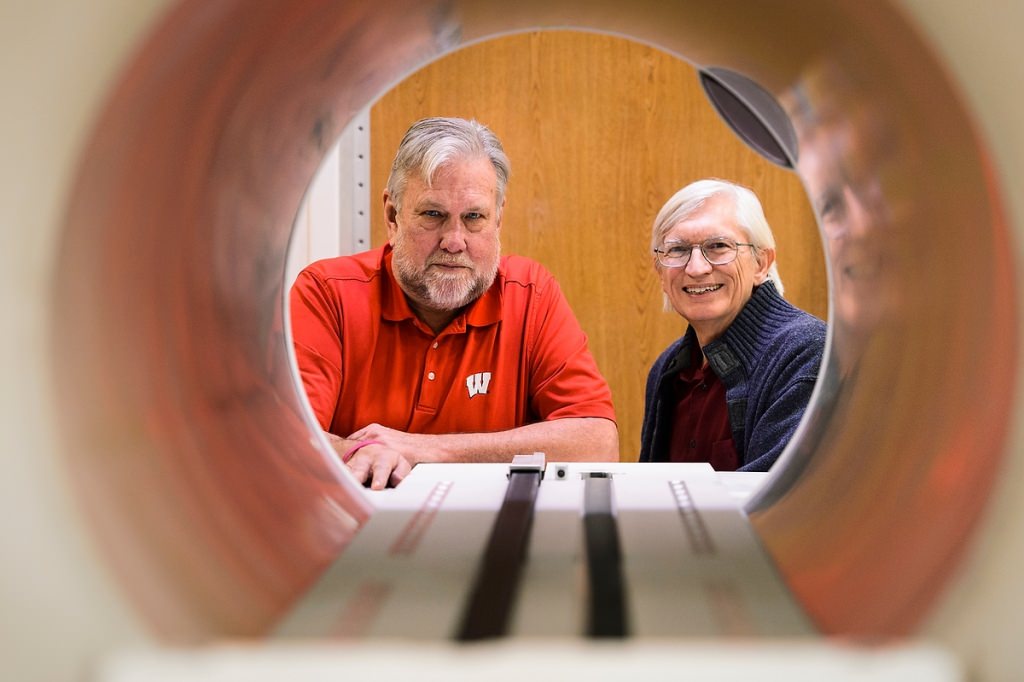
Frank Rath, left, a faculty associate in the College of Engineering, and Bruce Thomadsen, professor of medical physics, are pictured looking through the opening of a piece of radiotherapy treatment equipment at the Carbone Cancer Center. Thomadsen and Rath helped found the Center for the Assessment of Radiological Science as a way to help monitor and improve incidents of radiation-treatment safety in health care. Photo: Jeff Miller
A patient preparing for cancer treatment that uses radiation has plenty to worry about. Getting the right treatment every time — just the right dose in just the right place — should be taken for granted. And yet in radiotherapy, as in every other human activity, errors happen.
Tracking down and eliminating errors in a way that simultaneously prevents further problems is the stock-in-trade of the Center for the Assessment of Radiological Sciences, an organization born at the University of Wisconsin–Madison in 2012.
“The goal is to work with our clients, who sign a contract to enable this relationship,” says founding director Bruce Thomadsen, professor of medical physics at UW–Madison. “If an issue is reported related to the size or placement of a radiation dose, or other aspect of a treatment, we work with the client, going through all the data we have collected about the event.”
CARS incorporates reports from member hospitals and clinics into its database, says Thomadsen. “These incidents aren’t common, but they do happen, and there’s no sense in pretending otherwise.” CARS does not exist to exact punishment or enforce legal sanctions, but to understand and prevent, says Thomadsen. The professor has spent his 46-year career in the safety of medical devices that emit radiation and has just become president-elect of the American Association of Physicists in Medicine.
In their quest to found a center of excellence in radiation treatment, Thomadsen and Rock Mackie, a professor emeritus of medical physics, collaborated with Frank Rath, a faculty associate in the College of Engineering. Rath has expertise in the techniques, tools and methods for improving quality and safety in complex technology. He calls himself “the risk-assessment guy on campus. I use industrial tools to improve process quality and safety.”
At CARS, these tools are used in a “root-cause analysis of the incident,” says Thomadsen. “We discuss what we think is the underlying cause, and start a discussion with the client on how to improve quality.”
Simple radiation sources and procedures ruled the field of treatment for cancer and some other diseases a century ago, Thomadsen says. “Radiation therapy was at the forefront of quality assurance in medicine because medical physicists had to calibrate their equipment before practitioners in other disciplines did, but somehow our quality assurance got stalled with a focus on the equipment. Eventually we figured out that the leading cause of incidents was what people did — or didn’t do.”
Whether modern radiosurgery is performed with a radiation beam or an implanted source that undergoes radioactive decay inside the body, treatment is planned and controlled via software. Multiple people take part in prescribing and administering the dose, which raises the possibility of communication errors.
Thomadsen stresses that CARS can only improve the field if those who report have no fear of retribution. Information in the database that identifies facilities or patients is off limits to liability lawyers. Although at least one Wisconsin hospital takes part, the membership roll is private.
Evidence of what can go awry emerges from reports to CARS or the Nuclear Regulatory Commission’s Advisory Committee on the Medical Uses of Isotopes, says Thomadsen, who chaired the advisory committee from 2013 to 2015. Treatment planning is a common concern. “For example, a planner may digitize the path that the radioactive source travels through the patient in a different direction from what the computer was expecting, which can confuse the software and change how the treatment is carried out.”
Assessing the harm due to “events” in radiation treatment is “a very hard question,” says Thomadsen, who notes that only serious events must be reported. “When I was with the NRC’s advisory committee, we looked into the question in 2010 and found that serious errors occur about 0.01 percent of the time … which is pretty good, especially since most of those events did not result in harm to the patient.”
However, errors — defined as “the little failures that can lead to an event” — are very frequent, Thomadsen adds. Various studies, including several done in the UW–Madison Department of Industrial and Systems Engineering, find error rates of about two per emergency room visit. “Most of these are inconsequential, but getting a better handle on errors, and finding new ways to eliminate them, is a key goal of CARS.”
Eventually, the database may move beyond the current focus on radiation treatment to diagnostic radiation, like X-rays and CAT scans. A second advance could marshal a “knowledge-based learning system” to the task of preventing problems, says Rath. “We talk about taking this incident reporting system to the next level, so it can learn from incidents, from problems in the clinic, and become able to issue early warnings. We envision sharing this data with equipment vendors to accommodate safety improvements.”
The existing incarnation of CARS has identified problems in “plain vanilla” areas like scheduling. At one clinic, patients tended to arrive in bunches, causing overwork and some near misses, Thomadsen says. “They were staffed adequately on average, but understaffed in very busy periods. If you looked at one incident, you would not pick up the theme. But once you look at several incidents, you would see the patterns underlying these problems.”
