Powerful new genetic screening tool uses pathogens to probe infectious process

Researchers at the University of Wisconsin–Madison have used the gene editing technology CRISPR-Cas9 in a new way to identify human genes exploited by the influenza A virus. They have not only begun to identify more human genes that can inadvertently aid the virus in its pursuit to multiply within our cells, but they have also developed a method for probing the interplay between human cells and all manner of pathogens that can infect them. iStock / DrAfter123
As many as 2,800 genes may help shape interactions between human cells and influenza virus over the course of an infection, but scientists have so far identified only around a quarter of them. This leaves much of the infectious process shrouded in obscurity, posing a challenge to researchers on the hunt for better antiviral treatments.
Now, using the gene editing technology CRISPR-Cas9, a team at the University of Wisconsin–Madison has developed a new tool for ferreting out these obscured genes that the influenza A virus exploits for its own replication.
In doing so, the researchers have not only begun to identify more human genes that can inadvertently aid the virus in its pursuit to multiply within our cells, but they have also developed a method for probing the interplay between human cells and all manner of pathogens that can infect them.
The new tool is a twist on an established molecular biology technique known as CRISPR screening. Scientists have for years used CRISPR screens to understand how specific genes are involved in various biological functions. A traditional way to accomplish this is to remove specific gene sequences from cells and then observe the effect caused by the loss of those sequences.
While the screens are useful, their power for identifying genes’ functions has limits, particularly in the context of studying viral infections. Traditional screens require modifying human cells prior to infecting them, which could color any interpretations. So-called knockout screens can also miss the influence of some genes whose roles may be limited or redundant.
The UW–Madison team overcame these obstacles by engineering the influenza A virus to direct a different type of CRISPR-Cas9 screen. Instead of editing a genome, they used a version of CRISPR-Cas9 that activates human gene expression. They then designed an influenza virus to include genetic sequences that program Cas9, allowing the virus to act as both a director and subject of the screen.
The team then created a giant library of influenza viruses targeting every gene in the human genome and let them fight it out in a battle royale to see which viruses grew best and which were eliminated. Those that turned on genes essential for replication grew better, whereas those that turned on anti-viral properties were stopped. By looking at the genetic sequences in the winning viruses, the researchers could quickly identify human genes that aided replication. As an added benefit, because these viruses only carry part of the CRISPR machinery, this new screen only works in a lab.
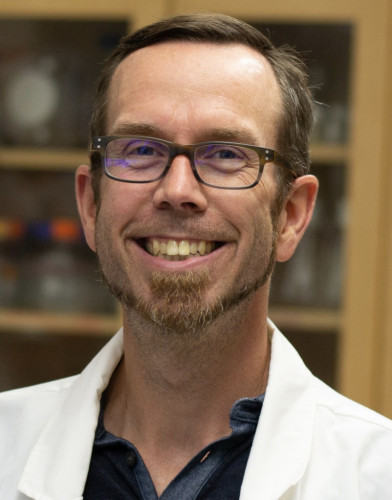
Andrew Mehle, a professor in the UW–Madison Department of Medical Microbiology and Immunology, guided work on the study.
“Viruses are the consummate cell biologists, ‘knowing’ exactly what pathways to exploit and which to avoid for a successful infection,” says Andrew Mehle, a professor in the UW–Madison Department of Medical Microbiology and Immunology who guided the work. “Our screen takes advantage of this to allow the virus itself to tell us which cellular genes have the biggest impact on replication.”
Using their new virus-directed screening tool, Mehle and his colleagues identified the enzyme TREX1 in human cells that inadvertently assists influenza A virus in its mission to replicate in cells.
Importantly, they learned that TREX1 doesn’t get involved in replication until well after the virus gains initial entry into a cell, shining a light on how the virus persists and multiplies during later stages of an infection. These stages aren’t as well documented as the initial infection, but knowing more about them could potentially lead to additional or more effective antiviral treatments.
“Finding any point along the way that we can manipulate is key to developing a multi-pronged approach to stop viral replication,” Mehle says.
The new tool is not limited to influenza A virus, either. Mehle says his group has already adapted it to explore the interplay between cells and other pathogens too, opening a door to investigating more stages of infection for many diseases caused by viruses and other microbes.

Publication of the study’s results are the culmination of then-postdoctoral researcher Cason King’s career. King died unexpectedly in August 2022 while preparing the manuscript.
Mehle and his colleagues described their development of the new technique and what it has initially revealed about influenza A virus infections in a paper that appeared in the Sept. 13 issue of the journal Cell Host & Microbe. The paper marks the culmination of lead author Cason King’s academic career. A senior postdoctoral researcher in Mehle’s lab, King died unexpectedly in August 2022 while preparing the manuscript.
“The paper is a true reflection of the great science Cason was doing, and the great scientist and friend he was,” says Mehle. “It would be understatement to say that the lab was devastated. Pushing this paper through and publishing it in such a high-profile journal has helped cement Cason’s impact and legacy.”
According to Mehle, the study is an example of the importance of research driven by open-ended hypotheses.
“Honestly, I was sitting in the office with a grad student and we were spitballing when I said, ‘I wonder if we can use influenza to program Cas9,’” Mehle says. “No real motivation or end goals. Just, ‘Can we do it? And, if we can do it, what questions can we ask?’”
Early indications suggests the answer is: quite a lot.
This research was supported by the National Institutes of Health (AI125897; AI164690), the Burroughs Wellcome Fund (Investigators in the Pathogenesis of Disease) and the UW2020:WARF Discovery Initiative (AI007414; GM140935; GM007215; AI148669).
