Delirium linked to brain injury after severe surgery
In a new study published today [Dec. 5, 2019] in the journal Brain, researchers at the University of Wisconsin–Madison School of Medicine and Public Health have discovered that delirium following severe surgery may be associated with brain injury.
“For a long time it has been thought that delirium, a state of confusion that can arise in sick patients, may lead to dementia and long-term cognitive problems,” says study leader Robert Sanders, assistant professor of anesthesiology at the UW School of Medicine and Public Health. “However, it has been impossible to prove that delirium causes these problems, but our study directly links inflammation during delirium with nerve injury.”
Sanders and his team were able to demonstrate that delirium is associated with injury to nervous tissue in the brain that could lead to loss of cognitive ability. The findings could inform future efforts to educate patients about the risks of surgery, especially major surgery in patients older than age 65 years.
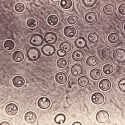
The research team demonstrated that a protein called neurofilament light, which indicates brain injury, increased in the presence of diagnosed delirium in patients following severe surgery. Delirium is an acute state of confusion that results in inattention and cognitive failure.
Researchers examined blood samples collected from 93 participants before and after surgery, to look for changes in neurofilament light and changes to markers for inflammation. The average age of study participants was 71.
Following surgery, 39 of the participants experienced delirium, particularly those who underwent vascular surgery or other higher-risk surgeries. All study subjects who underwent surgery saw an increase in their levels of neurofilament light, but the increase was profound in the group whose members experienced delirium.
In fact, the researchers found that as delirium severity increased, so did the amount of the neurofilament light protein and signs of inflammation in the blood of participants. They also found that neuronal injury was associated with increases in delirium severity, regardless of inflammation.
The proportional change of neurofilament light with severity of delirium provides further information to support a causal link of delirium and brain injury, Sanders says.
“However, we don’t yet know for certain whether there is a cause-and-effect relationship between these changes in neurofilament light and long-term changes in cognition,” he adds. “We also don’t know whether they are related to onset of dementia. Further research is needed.”
Future studies should explore the severity of any subsequent cognitive decline, says Sanders.
“We recommend a study that examines a large observational group, or registry of studies, that explores all the possible causes of delirium to confirm our observations, identify the role of neuronal injury in inflammation-driven delirium, as well as other causes, and to link to long-term cognitive outcomes,” he says.
The study was funded by grants NIH K23 AG055700, R01 AG063849-01 and NHBLI 5T32HL091816-07.